Introduction
Texas penalties hit $2.3M.
Healthcare organizations across Texas are facing a crisis that threatens their financial survival. Your provider directories are probably wrong right now - and you might not even know it.
Provider directory inaccuracies plague health plans nationwide, creating frustrated members, operational chaos, and penalties that can destroy organizations. Recent studies reveal that up to 50% of provider directory listings contain outdated or incorrect information.
This leaves your members unable to access the care you promised them.
Even worse, both state and federal regulators are now imposing severe financial penalties on organizations that can't keep their directories accurate.
Texas State Laws Governing Provider Directory Accuracy
Texas Law: 15-Day Update Rules
Texas Insurance Code Chapter 1301 takes provider directory accuracy seriously. You have 15 business days to update provider status changes after notification. Miss that deadline? You're facing violations that can cripple your organization.
The financial consequences are staggering. Texas regulators impose penalties ranging from $25,000 for minor violations to over $1 million for repeated non-compliance.
Here's a real scenario: You're managing directories for a mid-sized health plan when a popular orthopedic surgeon leaves your network. If you don't update your directory within 15 days, every member who calls that office represents a potential violation. That's 200+ members calling a disconnected number, each representing a separate compliance failure.
The Texas Department of Insurance conducts regular audits using mystery shopper programs and member complaints as trigger events. When they find problems, the penalties come fast and hit hard.
In 2024 alone, three major insurers received combined penalties exceeding $2.3 million for directory violations. These cases involved outdated provider addresses, incorrect specialty listings, and failure to remove terminated providers within required timeframes.
State-Specific Directory Standards
Texas demands comprehensive provider information beyond basic contact details. Your provider directories must include office hours, languages spoken, accessibility features, and whether providers accept new patients. Texas SB 1003 directory requirements expanded these mandates significantly.
Here's what makes Texas different from other states: the quarterly verification process demands documented outreach to every single network provider. You need call logs, email confirmations, and attestation forms as proof. Missing documentation during audits triggers automatic penalties regardless of whether your directory is actually accurate.
Consider this reality - maintaining a provider directory in Texas is like managing a massive phone book that changes daily, where you're legally required to prove you called everyone quarterly to verify their information is still correct.
Texas also requires real-time updates for high-impact changes:
- Provider terminations must appear within 48 hours
- Address changes need immediate updates
- Specialty modifications require same-day posting
Traditional manual processes simply can't keep up with this pace.
That's where HealthyFort Services makes the difference. Our tech-driven compliance tracking monitors Texas state law changes and ensures your directories meet every mandate without the manual headaches that lead to violations.
Federal No Surprises Act Compliance Requirements
Provider Directory Provisions Under the Act
The No Surprises Act transformed directory compliance starting January 2022. Now you must update directories within 48 hours of receiving provider information changes. No exceptions. No grace periods.
The Act also mandates provider verification every 90 days through direct contact or electronic confirmation. For large networks, this means thousands of verification contacts monthly. CMS No Surprises Act provider requirements specify exact documentation standards you must follow.
Federal penalties reach $25,000 per violation. Here's the concerning part - violations are calculated per affected member, not per incident. A single outdated provider listing that misleads 100 members could trigger $2.5 million in potential penalties.
The No Surprises Help Desk processes member complaints that frequently trigger enforcement investigations. When members can't reach providers listed in your directory, they file complaints. Those complaints become federal violations with your organization's name on them.
Recent enforcement data shows CMS assessed over $15 million in penalties during 2024. The average penalty per organization exceeded $800,000, reflecting how serious compliance failures have become.
What's driving these enforcement actions? Member frustration has reached a tipping point. When someone needs urgent care and calls five providers from your directory only to find disconnected numbers or full practices, they're not just annoyed - they're filing federal complaints.
Integration with State Law Requirements
You can't choose between federal and state compliance - you need both. Healthcare organizations must simultaneously satisfy No Surprises Act requirements and Texas state law mandates. This creates complex compliance situations that trap unprepared organizations.
While federal law requires 48-hour updates, Texas law demands 15-day updates for different trigger events. You need dual tracking systems to manage both requirements without missing deadlines.
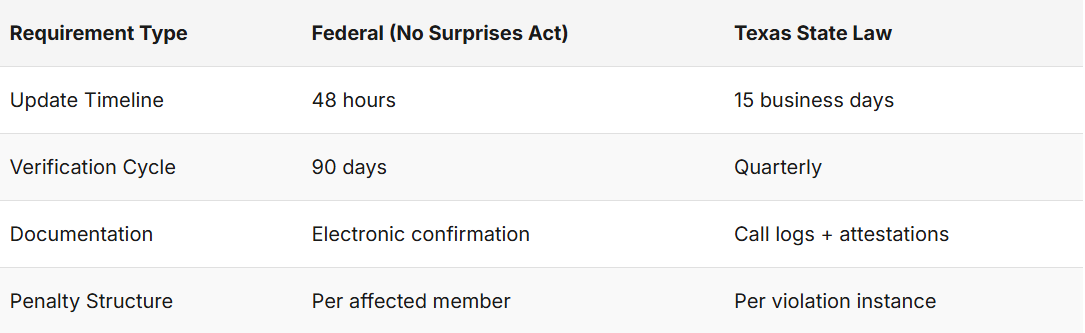
The documentation burden multiplies when satisfying both frameworks. Federal auditors expect 90-day verification cycles with specific contact methodologies, while Texas auditors require quarterly verification with state-approved documentation formats.
Think about trying to manage two different calendars with overlapping deadlines, different documentation requirements, and separate audit processes. That's the reality for Texas healthcare organizations today.
HealthyFort Services eliminates this complexity by managing both federal and Texas state requirements through a single integrated platform. You get compliance with both regulatory frameworks while maintaining complete audit documentation for each jurisdiction.
CMS Penalties and Enforcement Actions
CMS has shifted from warnings to penalties that can devastate organizations financially.
The base penalty of $25,000 per violation escalates based on severity, scope, and how your organization responds to compliance failures. Becker's coverage of CMS enforcement shows average penalties now exceed $1 million per case.
Here's a real example that should concern every healthcare administrator: A regional health plan received a $3.2 million fine for directory failures affecting over 150,000 members. The case involved outdated provider listings that remained uncorrected for eight months despite member complaints. CMS investigators found their manual verification processes had completely broken down.
What triggers these audits?
- Member complaint patterns
- State regulatory referrals
- Routine compliance reviews
- Data analytics identifying suspicious patterns
CMS uses advanced data analytics to identify organizations with higher-than-average complaint rates or unusual directory patterns. The HHS OIG audit reports frequently cite directory failures as indicators of broader operational problems.
When CMS audits begin, the documentation requirements are extensive. You must produce verification call logs, email confirmations, provider attestations, and system update records covering the entire audit period. Missing documentation results in presumed violations - guilty until proven innocent.
The appeals process requires detailed remediation plans and ongoing compliance monitoring. Organizations that successfully appeal penalties must demonstrate process improvements and sustained compliance over 12-month periods. Few organizations even attempt appeals due to the extensive documentation requirements and low success rates.
You might be wondering: "How do we know if we're at risk?" If your organization relies on manual directory updates, quarterly verification backlogs, or spreadsheet tracking, you're already in the danger zone.
Directory Verification Best Practices
Tech-Driven Verification Systems
Modern compliance demands automated systems that work around the clock. API integrations with CAQH ProView provide real-time provider data updates, eliminating the manual data entry errors that create violations.
Automated phone verification systems contact thousands of providers daily, validating contact information through interactive voice response technology. These systems generate compliance documentation automatically while identifying providers who need manual follow-up.
Address validation services integrate with NPPES/NPI Registry data to verify provider locations and practice details. When systems cross-reference multiple data sources, they flag discrepancies before you publish incorrect information.
Claims data integration provides powerful verification by identifying providers who haven't submitted claims within specified timeframes. This helps you spot inactive providers who won't respond to traditional verification attempts.
Here's what happens when you don't use these tools: Your verification team spends weeks calling providers manually, missing deadlines while creating compliance gaps that auditors will find.
Manual Verification Processes
Some verification still requires human contact, especially for high-risk providers and complex practice arrangements. Standardized phone verification scripts ensure consistent data collection while meeting regulatory documentation requirements. Provider verification templates from CMS provide compliance-ready documentation formats.
Non-responsive provider protocols must balance regulatory requirements with practical limitations. Most organizations allow 30 days for initial response, followed by certified mail requests and final termination procedures. You must document every single outreach attempt for audit defense.
Consider this scenario: Dr. Martinez hasn't responded to three verification attempts. Your team needs clear escalation procedures that involve credentialing departments and supervisor review. Clear escalation timelines prevent compliance violations while ensuring data accuracy.
High-volume verification periods around regulatory deadlines require surge capacity planning. Many organizations struggle when quarterly verification requirements coincide with credentialing renewals and routine provider updates.
What happens when verification backlogs build up? You're looking at systematic compliance failures that take months to resolve and cost hundreds of thousands in penalties.
Technology Solutions for Compliance
Spreadsheet tracking methods fail under modern regulatory pressure. Version control issues, limited collaboration capabilities, and lack of automated alerts make them compliance disasters waiting to happen.
HL7 FHIR US Core standards provide API-driven directory updates that maintain data consistency across multiple platforms. Real-time synchronization ensures directory updates appear across member websites, provider portals, and customer service systems simultaneously.
Compliance dashboards provide real-time visibility into verification status, pending updates, and regulatory deadline tracking. These tools help compliance teams prioritize work and identify potential violations before they occur.
HealthyFort Services provides technology solutions that automate the entire verification workflow, from provider outreach through compliance documentation. Our platform eliminates manual processes while ensuring both Texas state law and federal compliance requirements are consistently met.
Common Directory Management Pitfalls
Healthcare organizations consistently make five major mistakes that lead to compliance disasters.
First mistake: Relying on manual processes that can't scale. Studies show directory inaccuracies persist even after regulatory enforcement increased. Manual tracking simply can't keep up with modern requirements.
Sarah, a compliance manager at a 500-provider network, spent 40 hours weekly just tracking verification deadlines in spreadsheets. When audit season arrived, she couldn't produce the required documentation for 30% of providers. The result? A $400,000 penalty that could have been avoided with proper systems.
Second mistake: Operating siloed systems that create data chaos. When credentialing, claims, and directory management operate independently, provider information updated in one system may not reach member-facing directories for weeks.
Third mistake: Incomplete provider onboarding that skips required data elements. New providers begin seeing patients before their directory listings include required accessibility information, languages spoken, or new patient acceptance status.
Fourth mistake: Ignoring quarterly verification requirements that create cascading failures. The payer case study on directory compliance shows how verification backlogs create compliance problems that take months to resolve.
Fifth mistake: Under-resourcing directory management as a secondary priority. Compliance teams often lack adequate staffing or technology resources to maintain required verification schedules, leading to failures that trigger enforcement actions.
Directory management operates like air traffic control. You can't afford mistakes, delays, or system failures when lives and millions of dollars are at stake.
Conclusion
Your provider directories have become regulatory minefields where mistakes cost hundreds of thousands of dollars in penalties.
The dual compliance requirements under Texas state law and the No Surprises Act demand automated solutions that traditional manual processes simply cannot provide. Organizations that continue relying on outdated approaches face inevitable compliance failures.
Think about this: While you're reading this article, your directories are probably becoming less accurate. Providers are changing addresses, leaving networks, and updating their practices. Every delay in updating these changes creates potential violations.
HealthyFort Services offers directory management solutions that ensure compliance while letting you focus on patient care instead of administrative nightmares. Contact us to learn how automated directory management can protect your organization from regulatory penalties while improving member satisfaction.
FAQs
What are the specific Texas state law requirements for provider directory updates?
Texas Insurance Code Chapter 1301 requires provider directory updates within 15 business days of status changes, quarterly verification of all network providers, and inclusion of specific data elements like office hours and accessibility features.
How do No Surprises Act requirements differ from Texas state law?
The No Surprises Act requires 48-hour updates for provider changes and 90-day verification cycles, while Texas law mandates 15-day updates and quarterly verification. You must comply with both sets of requirements simultaneously.
What triggers a CMS audit of provider directory compliance?
CMS audits are triggered by member complaint patterns, state regulatory referrals, routine compliance reviews, and data analytics that identify unusual complaint rates or directory discrepancies.
What documentation is required to prove directory compliance during audits?
Auditors require verification call logs, email confirmations, provider attestations, system update records, and documentation of non-responsive provider outreach attempts covering the entire audit period.
How can healthcare organizations automate directory compliance processes?
Organizations can implement API integrations with CAQH ProView, automated verification systems, real-time data synchronization, and compliance dashboards to reduce manual processes and ensure consistent regulatory compliance.
What are the financial penalties for directory compliance failures?
Texas penalties range from $25,000 to over $1 million per case, while federal penalties reach $25,000 per violation calculated per affected member, with recent enforcement actions averaging over $800,000 per organization.
How often must providers be contacted for directory verification?
The No Surprises Act requires provider verification every 90 days, while Texas law mandates quarterly verification, essentially requiring monthly verification activities to maintain compliance with both frameworks.