Introduction — Why this guide matters
You're losing revenue.
Revenue cycle management, RCM, AR follow ups, and insurance and benefit verification leak cash.
This guide shows a practical 4C framework and short pilots you can run in 60–90 days to reduce denials and speed payments.
Table of contents:
- The hidden costs of inefficient operations
- Framework overview — The 4C RCM Framework
- Capture
- Control
- Chase
- Comply
- Implementing the 4C Framework — Practical steps
- Step 1: Assess current state and prioritize fixes
- Step 2: Build automation and workflow rules
- Step 3: Choose a partner or run internally
- Common mistakes and how to avoid them
- How smart service partners solve this
- Faster cash flow through managed AR
- Reduced denials through payer expertise
- Compliance, provider data, and audit readiness
- Two short, real-feeling anecdotes
- Conclusion — Key takeaways and next step
- FAQs — Common questions
Start with a 30-day eligibility sample to see baseline issues quickly.
The hidden costs of inefficient operations
Denials, slow collections, and failed verifications add up fast. Many mid-sized hospitals see denial rates in the 5–12% range and days in AR often drift past 45–60 days. Those numbers are not just metrics — they are cash that’s not hitting the bank.
Failed insurance and benefit verification is one of the largest avoidable causes. If front-line staff miss coverage limits, prior authorization needs, or secondary payer data, claims are denied as ineligible. Each denied claim spawns rework: coders re-open charts, clinicians supply records, and billers file appeals. That rework costs time and money.
Downstream effects multiply. Staff burnout grows as teams chase exceptions. Patients get frustrated by surprise balances. Compliance risk rises when provider data or credentialing records don’t match during audits.
A short scenario: Dr. Sarah’s hospital averaged a 9% denial rate in one quarter. Pre-service benefit misses drove 35% of those denials. Over three months the hospital saw a 22-day rise in days in AR and a cash shortfall that paused planned purchases. That lost revenue could have funded a care coordinator and upgraded scheduling tools.
Concrete math makes the point. A 200-bed hospital with $120M annual gross charges and a 9% denial rate loses roughly $10.8M in billed value before appeals. Recovering half of avoidable denials — even after write-offs and adjustments — can free several hundred thousand dollars per quarter. That’s not theory. It pays for staff and for tools that stabilize operations.
The opportunity cost is real. Recovering even half of avoidable denials frees funds for staffing, technology, and patient services. Think of RCM fixes as a reclaimed revenue stream you can re-deploy.
Framework overview — The 4C RCM Framework
The 4C Framework keeps work focused and measurable. It covers Capture, Control, Chase, and Comply — front-end verification, claim preparation, prioritized AR, and governance.
Think of the framework as a relay race. Each team hands off to the next. When the handoff is clean, claims reach the finish line faster.
Capture: Accurate eligibility and benefits
Capture means validating insurance at scheduling and registration. Check primary vs. secondary payer, effective dates, prior authorization status, benefit limits, and estimated patient responsibility. Track these data points: policy number, plan code, subscriber relationship, authorization ID, and deductible met-to-date.
Quick validation sources: payer portals, employer benefits portals, and eligibility APIs that return coverage flags. If a patient lacks authorization, surface it at scheduling and cancel or reschedule rather than submitting a claim likely to deny.
Example: add a short scheduler checklist at registration. A two-item flag — “authorization required” and “secondary on file” — reduces same-day denials.
Capture is a front-loaded investment. It pays off downstream.
Control: Clean claims and payer rule checks
Control is about producing claims that match payer expectations. Use claim-edit rules for missing modifiers, invalid CPT/NDC pairings, and mismatched place-of-service codes. Map your top payer rules and prioritize the edits that drive the highest-dollar denials.
Keep a prioritized payer-rule library and log exceptions. If a rule repeatedly triggers, add it to training or automation so the first pass succeeds more often.
Example: map your top five payers and track the three edits that cause most denials. Fix those first.
A simple rule set can raise first-pass acceptance noticeably.
Chase: Prioritized AR follow-ups and cadence
Chase sorts AR by probability-of-recovery and age. Triage accounts into buckets: 0–30, 31–60, 61–120, 121+ days, and attach a cadence and owner to each. Assign high-probability accounts to collectors and complex denials to appeals specialists.
Track KPIs: collection rate, days in AR, denial overturn rate, and net collections. Use a risk score to route work automatically and focus human effort where it delivers the most dollars.
One-sentence test: if you’re spending the same effort on a $40 patient balance as on a $4,000 payer denial, reprioritize.
Comply: Provider data and audit readiness
Comply covers provider directory accuracy, credentialing sync, and retention of audit trails. Reconcile directory entries with credentialing records regularly. Keep timestamped logs for verifications, authorizations, and appeals.
Schedule periodic reconciliations and retain documentation to meet state and payer audits. Small gaps in provider data can trigger fines and call-center surges.
A quick rule: run a weekly directory reconciliation for high-volume service lines.
Implementing the 4C Framework — Practical steps
Step 1: Assess current state and prioritize fixes
Start with a revenue cycle audit. Map workflows from scheduling through cash posting. Note tools, handoffs, and common failure points. Interview schedulers, coders, collectors, and compliance staff to see where work piles up.
Measure denial reasons and the highest-dollar AR buckets. Run a 30-day sample of eligibility checks vs. payer responses to measure front-end accuracy. Use that sample to expose recurring misses: wrong plan codes, expired authorizations, or missing secondary insurance.
Create an action backlog. Score each task by estimated impact (dollars recovered) and effort (FTE hours or IT time). Prioritize quick wins: automate high-volume eligibility checks, add a front-end authorization checklist, and apply a top-10 payer-edit rule set.
Engage these stakeholders: finance, IT, billing, clinical leadership, and compliance. Form a short steering group for weekly 30-minute reviews during the pilot.
Quick action checklist:
- Map end-to-end RCM workflows.
- Run 30-day eligibility vs. payer response test.
- List top denial reasons and their dollar impact.
- Score backlog tasks by impact and effort.
- Assign owners and weekly review cadence.
One-sentence sprint: pick one service line and run the test.
Step 2: Build automation and workflow rules
Automate determinable tasks first. Implement eligibility checks at scheduling that flag coverage gaps and required prior authorizations. Add automated claim-edit rules for your top denial causes. Configure auto-corrections and exception queues when edits can’t be safely fixed.
Set up automated AR workflows that route tasks by risk score. Example cadence:
- 0–30 days: automated patient statement and payer follow-up.
- 31–60 days: collector outreach and payer escalation.
- 61–120 days: focused appeals and clinical documentation review.
- 121+ days: executive review for write-off versus continued pursuit.
Pilot with a single service line like outpatient surgery. It’s a repeatable, high-volume area where you can measure lift quickly.
Pilot KPIs table:
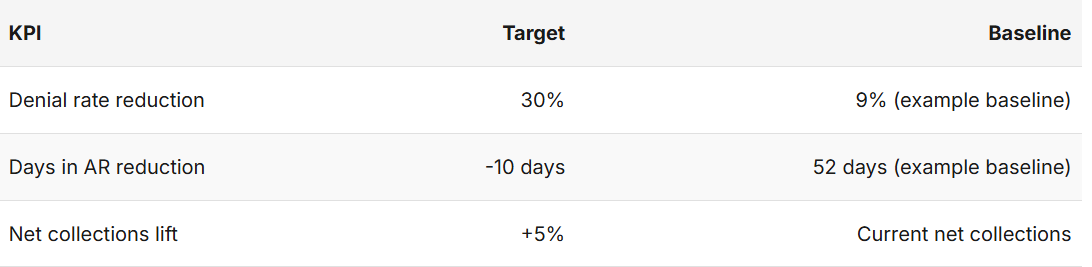
Keep human review for nuanced cases. Automation should free staff to handle complex appeals rather than push all work into opaque queues. Create an exceptions dashboard so teams can adjust rules without disrupting patients.
What to automate first: eligibility checks, top-10 payer edits, and simple AR triage. Automate low-risk corrections and route the rest to named owners.
Step 3: Choose a partner or run internally
Weigh trade-offs honestly. In-house RCM maintains control but requires investment in people, integrations, and payer knowledge. Partners offer scale and specialist staff, but vendor selection and governance are critical.
Partner selection criteria:
- Real metrics on denial reversal and collections lift.
- Proven integration experience with Epic, Cerner, and common billing systems.
- Transparent SLAs, reporting dashboards, and audit logs.
- SOC/HIPAA controls and clear documentation retention policy.
- Short pilot contracts (60–90 days) with data access.
Sample vendor evaluation questions:
- Can you show outcomes from a 60–90 day pilot on an outpatient surgery line?
- What gates and KPIs are included in the pilot termination terms?
- How do you provide raw data and audit logs at the end of the pilot?
Evaluate vendors with a 60–90 day proof-of-value pilot that includes data sharing and clear KPIs. Watch for contracting red flags: hidden per-claim fees, long lock-in without exit data, or vendors that refuse to provide audit logs.
When comparing options, ask for three things: a short, documented implementation plan, sample dashboards, and a pilot ROI model showing net dollars recovered versus fees.
HealthyFort Services can be evaluated against these criteria. It offers managed billing, claims tracking, payer administration, and provider directory management. Consider running HealthyFort in a pilot to test denial reduction and payment speed with transparent reporting.
Common mistakes and how to avoid them
Neglecting front-end verification and relying on retrospective fixes wastes resources. Front-end validation prevents the majority of avoidable denials.
Over-automation without exception handling is risky. If automation creates opaque queues, claims stall. Build clear exception circuits and assign human owners to those queues.
Avoid vendor black boxes. Demand dashboards and audit logs so your team sees what edits fired and why appeals were submitted. Don’t track only denial counts — measure denial recovery rate and net collections.
Prevent scope creep in pilots. Keep pilots narrow: one service line, set KPIs, and a 60–90 day timeframe. Use weekly feedback loops with clinical, billing, and payer teams to iterate quickly.
A short rule: require raw data access at contract signing.
How smart service partners solve this
Faster cash flow through managed AR
Good partners combine automation with specialist follow-ups. Automated triage finds high-probability accounts and directs collectors to the highest-yield tasks. Appeals specialists handle complex denials within payer windows so claims move faster through adjudication.
Practical example (hypothetical): a partner routes high-probability AR to senior collectors and files targeted appeals within 10 days, reducing days in AR by double digits for that service line.
HealthyFort’s managed AR offering pairs automated prioritization with specialist appeals to shorten payment cycles without adding internal headcount.
Reduced denials through payer expertise
Partners that maintain payer-rule libraries and historical denial patterns can raise first-pass acceptance. They code to payer expectations and tailor appeals language to each payer’s known preferences.
When you evaluate vendors, ask for case studies that show denial reduction percentages and the specific playbook used. This clarity separates vendors who fix symptoms from those who fix root causes.
HealthyFort’s payer administration focuses on mapping payer rules and applying automated edits plus manual reviews for exceptions — a combined approach that increases first-pass success.
Compliance, provider data, and audit readiness
A partner should centralize provider directories, sync credentialing, and keep timestamped audit trails. Require vendors to produce SOC/HIPAA documentation and an implementation playbook.
Vendor checklist:
- API access for EHR and billing system integration.
- SLA for denial investigation and appeal submission.
- Regular performance reporting and dashboard access.
- Evidence of SOC/HIPAA controls and documentation retention.
HealthyFort includes provider directory management and retains claims documentation to help hospitals respond quickly to audits and regulator inquiries.
Two short, real-feeling anecdotes
Mini-case: eligibility check fixes At a mid-sized hospital, schedulers were missing authorization IDs for outpatient imaging. The team ran a 30-day eligibility vs. payer response sample, added a two-field check at registration, and retrained schedulers. Within six weeks same-day denials for imaging dropped by nearly 50%. Days in AR for that service line fell by 14 days in the first quarter.
Mini-case: prioritized AR workflow A clinic set up a prioritized collector worklist based on risk score. Collectors focused on the top 20 high-probability accounts each morning and escalated complex denials to appeals staff. Over one month they closed the most valuable outstanding accounts in one week instead of two months. Net collections rose and morale improved because staff saw tangible results.
These quick stories show how small fixes drive measurable change.
Conclusion — Key takeaways and next step
The 4C Framework — Capture, Control, Chase, Comply — gives a clear path to reduce hidden costs and improve cash flow. Small, targeted pilots around eligibility checks, claim edits, and prioritized AR deliver quick wins.
Start with a 60–90 day pilot on one service line. Measure denial rate, days in AR, and net collections. Evaluate partners against integrations, reporting, and transparency. Consider HealthyFort Services as a pilot option to test denial reduction and accelerate payments with clear KPIs and data access.
Run the 30-day eligibility sample now. See the problems and quantify the gains.
FAQs — Common questions Q1: How quickly can we expect reduced denials? — Often within 60–90 days with a focused pilot.
Q2: What KPIs matter most? — Days in AR, denial rate, net collections.
Q3: Should we automate everything? — No — automate high-volume checks and keep humans for exceptions.
Q4: How to measure partner ROI? — Compare incremental collections vs. fees over 90 days.
Q5: What integrations are essential? — EHR (Epic/Cerner), billing system, payer portals.
Q6: Is patient experience affected? — Yes — fewer billing errors improve satisfaction.
Q7: What simple test can I run this week? — Run a 30-day sample of eligibility checks vs. payer responses for one service line and score common misses.